Next Steps: Radiotherapy and Chemotherapy
Richard RaceThe plan for the next ~12 months.
Note: This is about my own experience. If you're reading this because you or someone you know has a brain tumour, don't assume it will be the same. And every major surgery carries risks - don't read into my own complex situation. This is for me to help process what has happened, what's happening and what's to come.
Why Radiotherapy and Chemotherapy if it’s not cancer?
As I stated in my previous post I have an oligodendroglioma Grade 2 (non-cancerous) and the next step:
…isn’t to eliminate the remaining tumour. It will be to stop it growing. It is currently inoperable due to the location and diffuse nature… If it shrinks that would be a bonus.
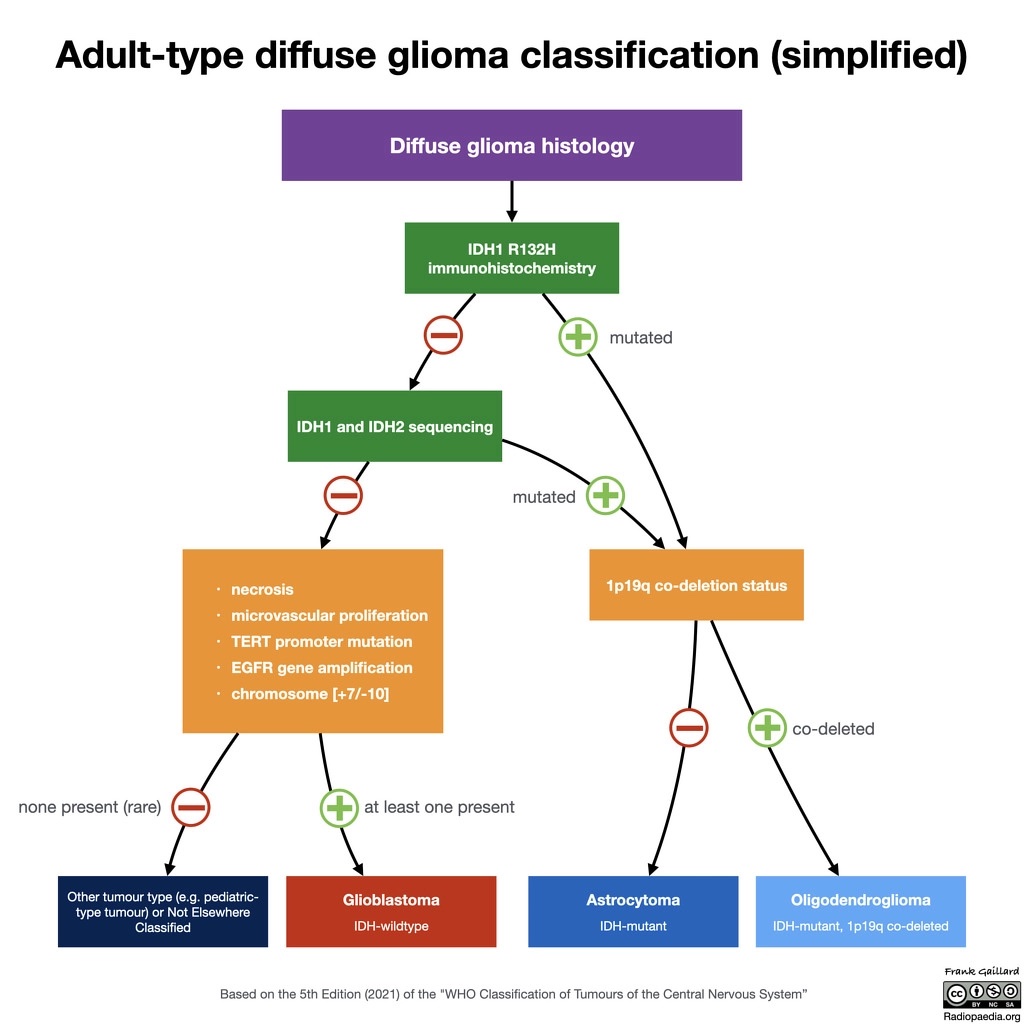
The good news is that oligodendrogliomas respond well to chemotherapy due to the genetic make up of the tumour cells. The World Health Organisation (WHO) defines the specific characteristics of brain tumours, the latest edition is from 2021. It tightens up the classifications from the previous editions1.
To be an oligodendroglioma it is required to have certain properties:
Glioma classifications showing the flow to diagnosis2
As oligodendrogliomas respond well to chemotherapy, due to the 1q/19q co-deletion3, it’s allowed to grow a little quicker than other types of brain tumours (for the purpose of grading). Since my tumour is rather large (~193cm3 before having the surgery to remove half of it) and diffuse (intertwined in my brain/inoperable). Radiotherapy followed by chemotherapy is the best course of action.
Critically, we want to stop my brain tumour to developing into a Grade 3 tumour. Actual cancer.
Radiotherapy:
The aim of radiotherapy is to treat the tumour that the neurosurgeons could not operate on. I’ll be starting soon - I actually have my planning session tomorrow.
There are various appointments needed for radiotherapy e.g. MRI and CT scans and a Mask Fitting.
This is an intensive treatment, it is every weekday for 6 weeks. The actual radiotherapy treatment per day will, for me, take less time than it will take for travel to/from the hospital.
The main side effects I’m expecting:
- Hair loss
- Fatigue during and up to 2 weeks after
- Brain swelling (I’ll have medication to help)
- Skin irritation (basically sun burn)
Chemotherapy:
I’ll start chemotherapy about 6 weeks after radiotherapy ends.
The goal of this treatment will be to kill any leftover fast-growing cells - to try to ensure that my brain tumour will hopefully not turn into a Grade 3.
The current plan is to have 6 cycles of PCV:
- 10 days taking various drugs
- 32 days off drugs
- Rinse and repeat
This equates to 252 days in total of just chemotherapy.
What does this mean?
For the best part of the next year I’ll be having cancer treatment as a pre-emptive measure to ensure that I don’t actually get cancer. It’s driven by the size of the tumour, what’s left is inoperable and left untreated it will turn cancerous.
Another way of looking at it, is that I’m having palliative care/treatment. It’s goal is to maximise my qualify of life and extend my life as much as possible. There is not a cure for any brain tumour.
It’s important to note that being offered palliative care does not necessarily mean end of life is approaching. Palliative care should be offered when a person is first diagnosed with a serious illness to ensure they experience the best quality of life.4
Further reading:
https://www.macmillan.org.uk/cancer-information-and-support/treatments-and-drugs/pcv
Footnotes
-
https://onlinelibrary.wiley.com/doi/full/10.1111/bpa.13062 ↩
-
https://radiopaedia.org/cases/diffuse-glioma-classification-who-5th-edition-2021?lang=gb ↩
-
https://oncologypro.esmo.org/education-library/factsheets-on-biomarkers/1p-19q-co-deletion-in-glioma ↩
-
https://www.thebraintumourcharity.org/brain-tumour-diagnosis-treatment/treating-brain-tumours/adult-treatments/palliative-care-adults/ ↩